Melanoma and Other Skin Cancers Research Results and Study Updates
See Advances in Melanoma and Other Skin Cancers Research for an overview of recent findings and progress, plus ongoing projects supported by NCI.
In an event more than three decades in the making, FDA has approved lifileucel (Amtagvi), the first cancer treatment that uses immune cells called tumor-infiltrating lymphocytes, or TILs.
People with desmoplastic melanoma, a rare form of skin cancer, are likely to benefit from treatment with a single immunotherapy drug, pembrolizumab (Keytruda), according to new results from a small clinical trial.
For melanoma that can be treated with surgery, a few doses of pembrolizumab (Keytruda) beforehand looks to be a good choice. In a clinical trial, people who got the presurgical immunotherapy were much less likely to have their cancer come back than those who only received it after surgery.
Male patients with metastatic melanoma don’t live as long as females, and their tumors are more likely to become resistant to commonly used treatments. A new study may help explain why: the androgen receptor.
Regular skin cancer screening leads to many diagnoses of very early-stage melanomas, results from a new study suggest. The results add to a debate about whether screening is fueling an overdiagnosis of melanoma in the United States.
The immunotherapy treatment, which combines the LAG-3 inhibitor relatlimab and PD-1 inhibitor nivolumab, becomes the first new immune checkpoint inhibitor approved in 8 years. Both drugs are given to patients via a single infusion to treat advanced melanoma.
Melanoma cells that travel to the brain produce their own amyloid beta, helping the cells survive and form metastases, a new study in mice shows. The Alzheimer’s-linked proteins appear to tamp down the brain’s immune response to the cancer cells.
NCI researchers have found that a diet rich in fiber may help some people being treated for melanoma respond to immunotherapy treatment by influencing the gut microbiome. The new findings come from an analysis of people with melanoma and mouse models of the disease.
Clinical trial finds that ipilimumab (Yervoy) and nivolumab (Opdivo) combo is superior to a combination of the targeted therapies dabrafenib (Tafinlar) and trametinib (Mekinist) as the first treatment for metastatic BRAF-positive melanoma.
Trial results show patients who received the immunotherapy pembrolizumab (Keytruda) after surgery to remove high-risk stage II melanomas were less likely to have the cancer come back than those who received no treatment after surgery.
People with advanced melanoma treated with two immunotherapy drugs—nivolumab (Opdivo) and a new drug called relatlimab—lived longer without their cancer getting worse than those treated only with nivolumab, results from a large clinical trial show.
While doctors are familiar with the short-term side effects of immune checkpoint inhibitors, less is known about potential long-term side effects. A new study details the chronic side effects of these drugs in people who received them as part of treatment for melanoma.
In a large trial, tebentafusp helped patients with uveal melanoma live longer than patients who received other treatments for the disease. Uveal melanoma is an aggressive cancer of the eye, and many patients do not survive for a year once it has spread.
For patients with cancers that do not respond to immunotherapy drugs, the use of fecal transplants to modify the gut microbiome may help some of these patients respond to the immunotherapy drugs.
Melanoma cells that pass through the lymphatic system before entering the bloodstream are more resistant to cell death and spread more readily than cells that enter the bloodstream directly. The finding could lead to new treatment approaches.
After rising steadily for decades, the number of people in the United States who die each year from the skin cancer melanoma has dramatically dropped in recent years, results from a new study show. Learn what has contributed to the dramatic decline.
Melanoma cells that metastasize to other parts of the body produce high levels of a protein called MCT1, a new study in mice has found. Blocking MCT1 with an investigational drug, AZD3965, led to fewer and smaller metastatic tumors.
Researchers have developed a device that uses lasers and sound waves to scan circulating blood for melanoma cells. In a small study, the device accurately detected and reduced the amount of cancer cells in participants’ blood.
FDA has approved pembrolizumab (Keytruda) to treat people with Merkel cell carcinoma, a rare and deadly form of skin cancer. The approval covers use of the drug to treat locally advanced or metastatic forms of the disease.
The Food and Drug Administration approved the immunotherapy drug cemiplimab (Libtayo) for an advanced form of cutaneous squamous cell carcinoma (SCC), a common type of skin cancer. It is the first agent to be approved specifically for advanced SCC.
Results from a clinical trial show that the combination of nivolumab (Opdivo) and ipilimumab (Yervoy) halted the growth of or shrank metastatic brain tumors in more than half of participants with melanoma that had spread to the brain.
In a new study, NCI-led researchers developed a gene expression predictor that can indicate whether melanoma in a specific patient is likely to respond to treatment with immune checkpoint inhibitors, a type of immunotherapy.
A new study has linked age with how well patients with melanoma responded to treatment with immune checkpoint inhibitors. Experiments in mice suggested that the response pattern may be due to an age-related shift in the kinds of immune cells in tumors.
FDA recently approved the targeted-drug combination to treat patients with advanced melanoma and a subset of patients with a rare and aggressive form of thyroid cancer whose tumors have a specific mutation in the BRAF gene.
A new study suggests that patients with a rare form of melanoma, called desmoplastic melanoma, may be particularly likely to benefit from treatments known as immune checkpoint inhibitors. An NCI-sponsored clinical trial is already testing one such drug in patients with this cancer.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Skin cancer.
Paul Gruber ; Patrick M. Zito .
Affiliations
Last Update: May 14, 2023 .
- Continuing Education Activity
Skin cancer is the most common form of cancer in the United States and is generally classified as nonmelanoma skin cancer (NMSC) or melanoma. This activity provides a broad overview of skin cancer and reviews epidemiology, risk factors, pathogenesis, and treatment. This activity highlights the role of the interprofessional interprofessional team in managing patients with skin cancer.
- Identify the risk factors for the development of both nonmelanoma and melanoma skin cancers.
- Describe the common physical examination findings in actinic keratosis, squamous cell carcinoma, basal cell carcinoma, and melanoma.
- Summarize the treatment and management options available for skin cancer.
- Explain interprofessional team strategies for improving care coordination and communication in the management of skin cancer.
- Introduction
Skin cancer is the most common form of cancer in the United States. Skin cancer is generally classified as nonmelanoma skin cancer (NMSC) or melanoma. The exact incidence of skin cancer is difficult to determine due to the lack of diagnostic criteria and underreporting. However, several epidemiologic studies have shown an increasing incidence of both NMSC and melanoma over the past several decades. [1] [2] The diagnosis and treatment of these neoplasms represent a significant health problem from the standpoint of patient well-being and healthcare expenditures. Skin cancers are frequently located on the sun-exposed head and neck regions, which can result in significant morbidity during their diagnosis and treatment. Treatment options include surgical excision, cryotherapy, chemotherapy, immunotherapy, and radiation. Proper sun safety (i.e., sunscreen) is of the utmost importance to prevent skin cancer.
Ultraviolet (UV) solar radiation is the major etiologic factor in the development of cutaneous malignancies. An overwhelming majority of cases of NMSC and melanoma are related to UV exposure. [3] [4] UV exposure induces carcinogenesis by a twofold mechanism; it generates DNA damage that leads to mutation formation and reduces the ability of the host immune system to recognize and remove malignant cells. Basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) are the most common forms of NMSC, and both are derived from mutated epidermal keratinocytes. The cumulative lifetime UV exposure is directly correlated with the risk of developing BCC and SCC. Melanoma is the deadliest form of skin and is derived from mutated melanocytes. In contrast to BCC and SCC, the risk of developing melanoma is directly correlated with sun exposure during adolescence, specifically the number of sunburns aged 15 to 20. [5] Other risk factors implicated in the development of cutaneous malignancies include family history, chemical exposure, tanning bed use, human papillomavirus (HPV), Fitzpatrick skin type, the presence of melanocytic nevi, and immunosuppressed status. [6]
- Epidemiology
There are more skin cancers in the United States population than all other cancers combined. [7] These cancers are on the rise, representing a significant health problem from the standpoint of patient well-being and health expenditures. [8] Skin cancer occurs in all races worldwide. However, the risk is substantially higher in Whites due to the photoprotective effects of epidermal melanin. [9] In individuals with fair skin, approximately 75% to 80% of non-melanoma skin cancers are basal cell carcinomas, and up to 25% are squamous cell carcinomas. Heritable defects in DNA repair mechanisms, as seen in xeroderma pigmentosum and Muir-Torre Syndrome, also put afflicted individuals at high risk for cutaneous carcinomas.
- Pathophysiology
Sun exposure is the most important modifiable risk factor associated with the development of NMSC and melanoma. UV radiation can be subdivided into UV-A, UV-B, and UV-C. Sunlight is primarily composed of the UV-A (~90%) and UV-B (~10%) components. [3] UV-C rays are mostly absorbed by the atmosphere. UV-A has a longer wavelength (320-400 nm) and penetrates the dermis, causing the formation of free radicals. UV-B has a shorter wavelength (290-320 nm), penetrates to the level of the stratum basale of the epidermis, and causes the formation of thymine dimers. Both UV-A and UV-B contribute to carcinogenesis. However, UV-A is thought to play a larger role. UV radiation causes cell injury and apoptosis and impairs DNA repair mechanisms, leading to DNA mutations.
The development of cutaneous malignancy after DNA damage by solar radiation is multifactorial, including genetic factors, Fitzpatrick skin type, and immunosuppressed status. Most (90%) of cutaneous squamous cell carcinoma have UV-induced P53 gene mutations leading to the uninhibited proliferation of keratinocytes. [10] DNA mutations implicated in basal cell carcinoma include mutations in the PTCH gene and the p53 gene. [11] DNA mutations implicated in melanoma include mutations in cyclin-dependent kinase Inhibitor 2A (CDKN2A), melanocortin receptor 1 (MCR1), B-Raf, and DNA repair enzymes (e.g., UV-specific endonuclease in xeroderma pigmentosum). [12] [13]
- History and Physical
A thorough skin examination is useful to identify premalignant and malignant skin lesions. It is important to note the location, texture, size, color, shape, borders, and any recent change of suspicious lesions. Premalignant actinic keratoses often present as rough, gritty skin papules on an erythematous base. Basal cell carcinomas usually appear as pink pearly papules with telangiectasias. Squamous cell carcinomas are often pink, rough papules, patches, and plaques. Melanomas are characteristically brown-to-black lesions with asymmetry, irregular borders, color variegation, and diameters greater than 6 mm. Any new/changing lesion or lesion that appears different than other nevi on the body ("ugly duckling sign") is considered suspicious. [14]
Basal cell carcinomas and squamous cell carcinomas are commonly noted on parts of the head and neck that receive the most cumulative UV radiation over the course of a lifetime, such as the nose, ear, and upper lip. Melanomas can occur anywhere on the body and are most frequently discovered on the backs and shoulders of men and the lower limbs of women. [15] However, studies comparing the risk of melanoma per unit area of skin have found the face to be the highest risk area for melanoma. [16]
Evaluation of patients at risk for cutaneous carcinoma usually includes a full body skin examination by a medical professional. This can be done by most primary care providers; however, the evaluation is often performed by specialists with three years of post-medical school advanced dermatology training. The vast majority of concerning lesions on physical examination will undergo an office procedure called a skin biopsy. This is done under local anesthesia during an outpatient office visit. The specimen is then sent for special interpretation by a trained dermatopathologist. If the pathologist reading the tissue specimen under the microscope confirms the diagnosis of cutaneous malignancy, further intervention is usually warranted based on the pathologic diagnosis and clinical scenario.
- Treatment / Management
Treatment of precancerous lesions and cutaneous carcinoma should be tailored toward the individual patient scenario and the best clinical outcome. If presenting as isolated lesions, precancerous actinic keratoses can be treated with lesion-directed therapies such as cryotherapy. [17] Often, patients may present with numerous lesions and diffuse actinic damage, which requires field-directed therapy as opposed to individually treating each lesion. [17] This can be done with topical agents (5-fluorouracil, imiquimod, and ingenol mebutate) or with photodynamic therapy after sensitizing the skin with a topical agent. Initial pre-emptive efforts should be made to reduce the patient's risk profile for developing cutaneous carcinoma, including optimizing the immunosuppressant regimen in solid organ transplant patients, proper surveillance schedules in patients treated with immunomodulatory therapies and adequate therapy of precancerous lesions.
Basal cell carcinomas and squamous cell carcinomas, if superficial, can be treated with topical therapies depending on provider preference. However, the standard practice is to surgically treat these lesions with destructive means such as electrodesiccation and curettage or surgical excision. Skin cancers greater than 2 cm in diameter and those located on functionally and cosmetically sensitive sites (head/neck, hands, feet, genitalia) are usually referred for a special surgical procedure called Mohs micrographic surgery. [18] Some patients with aggressive and recurrent forms of basal cell carcinoma who are not good surgical candidates are treated with radiation therapy or systemic medications (e.g., vismodegib for basal cell carcinoma). [19]
Melanoma is the most aggressive and lethal form of cancer, and the gold standard of treatment is surgical excision. If caught early, surgical excision can be curative. Later stage tumors portend a poor prognosis and often require adjuvant chemotherapy or immunotherapy. [20]
- Differential Diagnosis
- Seborrheic keratoses
- Sebaceous hyperplasia
- Cherry angioma
- Benign melanocytic lesions
- Dysplastic nevus
- Metastatic tumors to the skin
- Epithelioid tumor
- Enhancing Healthcare Team Outcomes
Skin cancers are frequently encountered in clinical practice by the primary care provider, nurse practitioner, and internist. In all cases, the patient should be referred to a dermatologist for final confirmation. While the treatment of skin cancer is done by an oncologist and a dermatologist, the primary care providers play a vital role in prevention. Patients should be educated about avoiding too much sun, wearing appropriate garments when going outdoors, and applying sunscreen. Finally, patients should be educated on how to inspect their skin and when to seek medical assistance. [21]
- Review Questions
- Access free multiple choice questions on this topic.
- Access free CME on this topic.
- Click here for a simplified version.
- Comment on this article.
Disclosure: Paul Gruber declares no relevant financial relationships with ineligible companies.
Disclosure: Patrick Zito declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Gruber P, Zito PM. Skin Cancer. [Updated 2023 May 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review The epidemiology of skin cancer. [Dermatol Surg. 1996] Review The epidemiology of skin cancer. Gloster HM Jr, Brodland DG. Dermatol Surg. 1996 Mar; 22(3):217-26.
- Review Behavioral Counseling to Prevent Skin Cancer: Systematic Evidence Review to Update the 2003 U.S. Preventive Services Task Force Recommendation [ 2011] Review Behavioral Counseling to Prevent Skin Cancer: Systematic Evidence Review to Update the 2003 U.S. Preventive Services Task Force Recommendation Lin JS, Eder M, Weinmann S, Zuber SP, Beil TL, Plaut D, Lutz K. 2011 Feb
- Regional incidence of and reconstructive management patterns in melanoma and nonmelanoma skin cancer of the head and neck: A 3-year analysis in the inpatient setting. [J Plast Reconstr Aesthet Surg....] Regional incidence of and reconstructive management patterns in melanoma and nonmelanoma skin cancer of the head and neck: A 3-year analysis in the inpatient setting. Egeler SA, Huang A, Johnson AR, Ibrahim A, Bucknor A, Peymani A, Mureau MAM, Lin SJ. J Plast Reconstr Aesthet Surg. 2020 Mar; 73(3):507-515. Epub 2019 Nov 9.
- Behavior modification and risk perception in patients with nonmelanoma skin cancer. [WMJ. 2008] Behavior modification and risk perception in patients with nonmelanoma skin cancer. Rhee JS, Davis-Malesevich M, Logan BR, Neuburg M, Burzynski M, Nattinger AB. WMJ. 2008 Apr; 107(2):62-8.
- Review Epidemiology of skin cancer. [Adv Exp Med Biol. 2014] Review Epidemiology of skin cancer. Leiter U, Eigentler T, Garbe C. Adv Exp Med Biol. 2014; 810:120-40.
Recent Activity
- Skin Cancer - StatPearls Skin Cancer - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Skin cancer articles from across Nature Portfolio
Skin cancer can involve melanocytes, leading to melanoma, but there are other non-melanoma skin cancers. These include basal cell carcinoma, squamous cell carcinoma and, less commonly, Merkel cell carcinoma, Kaposis sarcoma and T-cell lymphoma of the skin.
Related Subjects
- Basal cell carcinoma
- Squamous cell carcinoma
Latest Research and Reviews
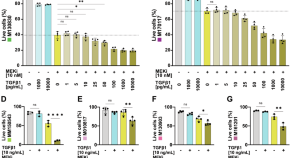
TGFβ signaling sensitizes MEKi-resistant human melanoma to targeted therapy-induced apoptosis
- Benjamin Loos
- Adrian Salas-Bastos
- Lukas Sommer
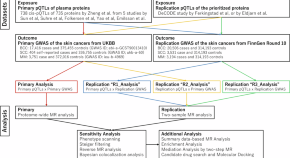
Systematic proteome-wide Mendelian randomization to prioritize causal plasma proteins for skin cancers
Our proteome-wide Mendelian randomization study prioritized plasma ASIP and CTSS as causal proteins of skin cancer risk, highlighting the possibility of identifying novel therapeutic targets and disease biomarkers.
- Masahiro Yoshikawa
- Tomohiro Nakayama
- Kensuke Asaba


Inhibition of glutaminase elicits senolysis in therapy-induced senescent melanoma cells
- Bryce Brunetti
- Akihiro Yoshida

Endothelial Pim3 kinase protects the vascular barrier during lung metastasis
The molecular regulation of endothelial cells (ECs) in metastasis remains unclear. Here, the authors use single-cell RNA-seq to examine the reprogramming of lung ECs in mouse models of melanoma metastasis, revealing that PIM3 protects capillary integrity and that its inhibition increases vascular leakage and metastatic colonisation.
- Niina M. Santio
- Keerthana Ganesh
- Pipsa Saharinen
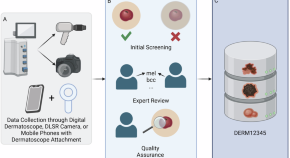
DERM12345: A Large, Multisource Dermatoscopic Skin Lesion Dataset with 40 Subclasses
- Abdurrahim Yilmaz
- Sirin Pekcan Yasar
- Burak Temelkuran
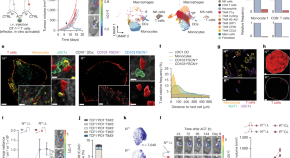
Cancer cells impair monocyte-mediated T cell stimulation to evade immunity
Inflammatory monocytes are identified as important players in T cell restimulation in the tumour microenvironment.
- Anais Elewaut
- Guillem Estivill
- Anna C. Obenauf
News and Comment
Identifying memory genes in cancer drug tolerance.
In this Journal Club, Chakrabarti discusses a method to dissect the molecular architecture of inheritable gene expression (memory) states that mark cells that transition into drug-tolerant persister cells in melanoma.
- Shaon Chakrabarti
Immunoproteasome as a biomarker for immunotherapy
In this Journal Club, Sabarinathan discusses a study suggesting immunoproteasome expression as a potential biomarker of response to immune checkpoint inhibition in melanoma.
- Radhakrishnan Sabarinathan

Male melanoma comes of age
In a recent study published in Cell , Chhabra et al. identify age- and sex-dependent changes in skin fibroblasts that drive melanoma aggressiveness, with aged male fibroblasts promoting a slow-cycling, invasive state and resistance to targeted therapy in melanoma cells.
- Daniela Senft
Leveraging the potential for deintensification in cancer care
Evidence-based reductions in cancer treatment that still preserve outcomes can result in an improved quality of life for patients and optimized healthcare resourcing. Using melanoma as an example, we define treatment deintensification, outlining barriers to its implementation, as well as existing guidance.
- Jennifer A. Soon
- Fanny Franchini
- Grant A. McArthur
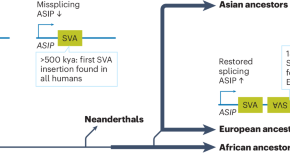
Mobile element insertions affect human pigmentation and skin cancer risk
Nearly 50% of the sequence of mammalian genomes is derived from mobile elements that inserted into the genome over millions of years of evolution. A recent mobile element insertion, found only in some individuals with European genetic ancestry, contributes to decreased skin pigmentation and increased sunburn frequency and skin cancer risk.
- Jeffrey M. Kidd

Carcinogenesis at single-cell resolution
In this study, Allan Balmain and colleagues used a mouse model to monitor stem cell networks at single-cell resolution during skin carcinogenesis, revealing two cancer stem cell states, rapid cycling and plasticity, between which cells can transition to drive tumour initiation, progression and therapy resistance.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Recent global patterns in skin cancer incidence, mortality, and prevalence
Affiliations.
- 1 Department of Dermatology, The First Hospital of China Medical University, Shenyang, Liaoning 110001, China.
- 2 NHC Key Laboratory of Immunodermatology, China Medical University, Shenyang, Liaoning 110001, China.
- 3 Key Laboratory of Immunodermatology, China Medical University, Ministry of Education, Shenyang, Liaoning 110001, China.
- 4 National and Local Joint Engineering Research Center of Immunodermatological Theranostics, Shenyang, Liaoning 110001, China.
- PMID: 39682020
- DOI: 10.1097/CM9.0000000000003416
Background: Skin cancer is a common skin disease whose incidence and mortality rates have been showing yearly increases. In this report, we update the most recent data on skin cancer as obtained from GLOBOCAN 2022.
Methods: The incidence and mortality rates of skin cancer (melanoma of skin and non-melanoma skin cancer) in GLOBOCAN 2022 were reviewed. These data were analyzed and the characteristics of incidence and mortality across five continents and top five countries in each continent are presented. In addition, correlations between Human Development Index (HDI) and age-standardized incidence and mortality rates of these two skin cancers are described.
Results: The GLOBOCAN 2022 data indicated that melanoma was the 17th most common cancer. An estimated 331,722 people were diagnosed with melanoma globally and approximately 58,667 died from this disease. For non-melanoma skin cancer, it ranks as the 5th most common cancer, and estimated 1,234,533 people were diagnosed with non-melanoma skin cancer globally and approximately 69,416 died from this disease. The incidence of skin cancer varies across geographic regions and countries, with a predominance observed in Oceania, North America, and Europe. Australia was ranked first in terms of incidence, while incidence rates in Africa and Asia were very low. Despite these regional differences in incidence, there was little geographic variation in mortality rates. Currently, the number of deaths from non-melanoma skin cancer exceeds that of melanoma of skin. HDI was positively associated with the incidence of both types of skin cancers, with a positive correlation obtained between HDI and mortality from melanoma of skin and a negative correlation between HDI and mortality from non-melanoma skin cancer.
Conclusions: Skin cancer remains a major disease burden worldwide. Substantial variations are observed across countries and regions with incidence rates being greater in Caucasians, the elderly, and in groups with prolonged exposures to ultraviolet rays. Further research on skin cancer will be required to provide a rationale for more effective preventions and treatments of this condition.
Copyright © 2024 The Chinese Medical Association, produced by Wolters Kluwer, Inc. under the CC-BY-NC-ND license.

IMAGES
COMMENTS
The Skin SPORE program's main focus is on melanoma research activities, but it also includes projects in other skin cancer types, such as cutaneous T-cell lymphoma. NCI's National Clinical Trials Network (NCTN) is a collection of organizations and clinicians that coordinates and supports cancer clinical trials at more than 3,000 sites across ...
Skin cancer has been the leading type of cancer worldwide. Melanoma and non-melanoma skin cancers are now the most common types of skin cancer that have been reached to epidemic proportion. Based on the rapid prevalence of skin cancers, and lack of efficient drug delivery systems, it is essential to surge the possible ways to prevent or cure ...
Journal of Skin Cancer is an open access journal publishing clinical and translational research on the detection, diagnosis, prevention, and treatment of skin malignancies. As part of Wiley's Forward Series , this journal offers a streamlined, faster publication experience with a strong emphasis on integrity.
This research paper introduces a comprehensive methodology to handle the complex issues related to skin cancer detection. This research presents a novel skin cancer recognition model based on ...
This survey is centred on categorizing research papers on skin cancer classification published in the last two decades, predominantly emphasizing machine learning and deep learning approaches ...
Find research articles on skin cancer, including melanoma, which may include news stories, clinical trials, blog posts, and descriptions of active studies. ... Regular skin cancer screening leads to many diagnoses of very early-stage melanomas, results from a new study suggest. The results add to a debate about whether screening is fueling an ...
Skin cancer is the most common form of cancer in the United States. Skin cancer is generally classified as nonmelanoma skin cancer (NMSC) or melanoma. The exact incidence of skin cancer is difficult to determine due to the lack of diagnostic criteria and underreporting. However, several epidemiologic studies have shown an increasing incidence of both NMSC and melanoma over the past several ...
Skin cancer can involve melanocytes, leading to melanoma, but there are other non-melanoma skin cancers. These include basal cell carcinoma, squamous cell carcinoma and, less commonly, Merkel cell ...
Melanoma is a serious skin cancer and has a rapidly rising incidence in many populations. 1 The incidence in White populations has increased by 3-5% per annum since the mid-20th century, with rates currently at 20-60 cases per 100 000 people per annum. 1 More commonly occurring non-melanoma skin cancers include squamous cell carcinoma and basal cell carcinoma, and together are increasingly ...
Background: Skin cancer is a common skin disease whose incidence and mortality rates have been showing yearly increases. In this report, we update the most recent data on skin cancer as obtained from GLOBOCAN 2022. Methods: The incidence and mortality rates of skin cancer (melanoma of skin and non-melanoma skin cancer) in GLOBOCAN 2022 were reviewed.